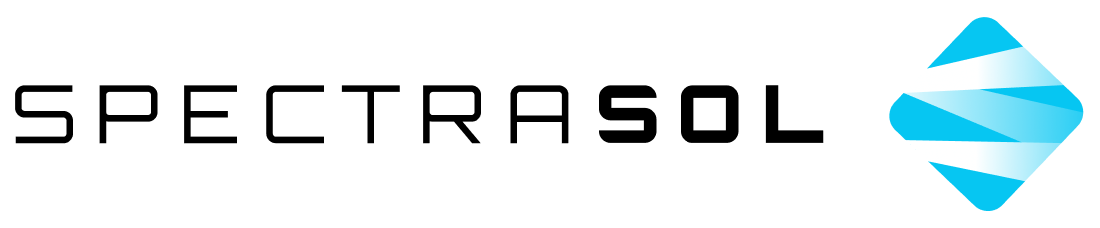
Should blue light and common LED sources raise concerns about retinal damage? Are current regulations sufficient? New studies from this year confirm the importance of LED light sources emitting full spectrum with sufficient red light.
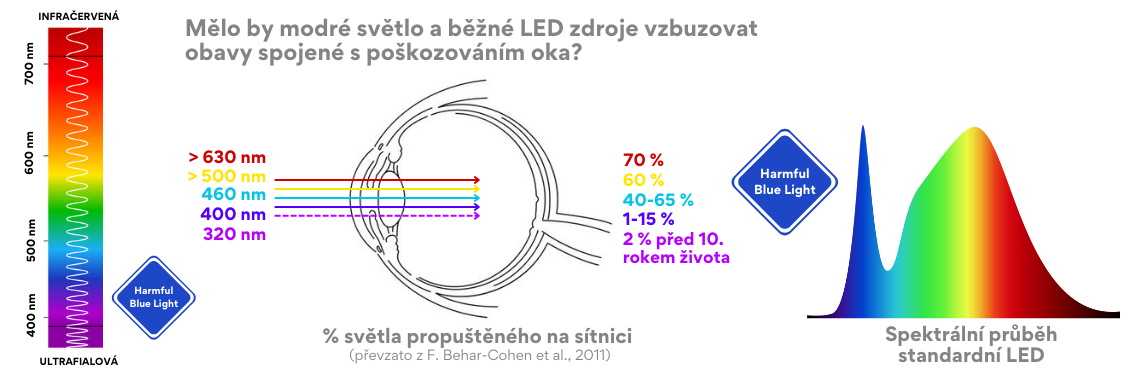
LED technology has significantly changed the light we are exposed to on a daily basis. Most LED lighting used indoors emits white light, which is produced by exciting a blue diode and covering it with a thin phosphor layer. The spectral distribution of the emitted light contains an intense peak in the blue spectral range with a maximum around 450 nm, a peak in the yellow-green spectral range, and typically very low emission in the red range (see Picture 1C). However, this spectrum is very different from the spectra emitted by traditional incandescent bulbs (tungsten, halogen, etc.), which have a high content of long (red) and a low content of short wavelengths (blue), see Picture 1A.
Currently, fluorescent lights remain the most common light sources in work and school environments. All of the mentioned types of light sources differ significantly from the spectral distribution of natural daylight, especially in the red and blue spectral areas (see Picture 1). The blue spectral range can be further divided into the so-called melanopic range, which is necessary for regulating our circadian rhythms (azure range), and the blue-violet range from 400-455 nm, often referred to as harmful blue light (HBL). As a result, the effects of blue light on organisms have begun to be studied, leading to regulations and guidelines concerning its safety with respect to potential retinal damage. High-intensity blue light acting for short periods is labeled as blue light hazard (BLH). But what about low-intensity blue light and prolonged exposure? New studies from this year provide answers by investigating the effects of white light and selected spectral areas on albino rats and human retinal pigment epithelial (RPE) cells.
Picture 1: Spectral power distribution (SPD) of various electrical light sources in comparison with natural daylight. A) Traditional incandescent bulb with intense emission in the red spectral range but low in the blue spectral range, B) Fluorescent light with dips in important spectral ranges (azure and red), C) Standard LED with intense emission in the harmful blue light (HBL) range, with a dip in the azure range and lack of emission in the red spectral range, D) Spectrasol LED with full-spectrum light, reduced emission in the HBL range, and adequate emission in both the azure and red spectral ranges, E) Natural daylight at noon.
Phototoxicity Threshold and Current Standards
Although ocular structures are protected by a complex antioxidant system and other defense mechanisms, excessive exposure to light, especially in the short-wavelength range, can cause irreversible damage to the retina. Light-induced retinal damage (photoretinitis) leads to the death of photoreceptors (rods and cones) and damage to retinal cells, particularly the retinal pigment epithelium (RPE), which is located beneath the photoreceptor layer and serves to recycle and degrade photopigments and also isolates the retina from the bloodstream, see Picture 2. RPE cells are therefore crucial for the survival of photoreceptors. Currently, blue light with a maximum around 455 nm is used to assess the phototoxicity of light sources. The threshold dose for primates’ retinas is 22 J/cm², and for rodents, it is 11 J/cm². The values established for primates formed the basis for current guidelines and standards: the IEC 62471 standard states that if the dose is less than 2.2 J/cm² over a period of 10,000 seconds (just under 3 hours), i.e., 1/10th of the phototoxicity threshold for primates, the light source is considered risk-free. Most light sources fall into this category and should not pose a risk to retinal damage. But is this really the case?
Picture 2: Retina Structure. The retina consists of several layers and different types of cells. The retinal pigment epithelium (RPE) is composed of RPE cells that are connected to the choroid through Bruch’s membrane, helping with recycling and degrading photopigments of photoreceptors (rods and cones). Image adapted from: S. Yang, J. Zhou, and D. Li, “Functions and Diseases of the Retinal Pigment Epithelium,” Frontiers in Pharmacology, vol. 12, July 2021, doi: 10.3389/fphar.2021.727870.
Is it really just blue light that causes retinal damage? And can red light help?
In the first study, albino rats were exposed to blue light (maximum at 450 nm). Even at a dose of 0.2 J/cm², immune cells infiltrated the retina, indicating an ongoing inflammatory response. DNA damage was also evaluated. At a dose of 0.5 J/cm², the number of damaged cells was up to 100 times higher than in the control group. There was also a loss of photoreceptors and changes in their morphology. These changes were observed even a week after exposure to blue light at a dose of 0.5 J/cm². Exposure to white light with a CCT of 2700 K and a total dose of 2 J/cm², with about 10% of the blue spectral area, caused 10 times more damage to retinal cells than exposure to blue light at the same dose (the dose of blue light in the white light was the same as the dose of monochromatic blue light: 0.2 J/cm²). These results suggest that other spectral areas must also play a role in photochemical retinal damage. This hypothesis was confirmed in a subsequent experiment where rats were exposed to green light with a wavelength of 507 nm. Compared to earlier sources, LED sources usually have significantly reduced emission in the red spectral area, and therefore, the effects of red light with a wavelength of 630 nm at a dose of 0.1 J/cm², white light at a dose of 0.9 J/cm², and the addition of red light to white light at a total dose of 1 J/cm² were further studied. The results are consistent with previous studies showing that red light has the potential to mitigate the harmful effects of blue light and partially protect against photoreceptor death, although statistical analysis showed no significant differences (a reduction in damaged cells by about a factor of 3).
The second study used similar methodologies. RPE cells derived from human induced pluripotent stem cells (hiPSC) were exposed to white light with a CCT of 3300 K and a dose of 3.6 J/cm². Although the phototoxicity threshold was set only for blue light, i.e., 22 J/cm², the dose of polychromatic light was significantly below this threshold. Calculating the proportion of blue light in the white light determined the blue light dose to be 0.185 J/cm², which is more than 100 times lower than the phototoxicity threshold, and yet there were changes in the overall cell structure, DNA damage, activation of cellular stress, and autophagy (a cellular process that maintains cellular homeostasis by recycling old or damaged cell components and proteins, serving as an emergency energy source in stressful conditions). Biochemical marker analysis revealed that blue light was likely responsible for the DNA damage, while red light seemed to induce modulation of DNA detection and/or repair mechanisms, including the inhibition of inflammatory processes.
Conclusion
The results of these studies suggest that the phototoxicity threshold for both rodents and primates should be stricter because even significantly lower doses caused eye damage. It appears that retinal damage is caused not only by blue light but also significantly by green light. Based on the same methodologies for determining phototoxicity thresholds for rodents and primates, it can be assumed that the phototoxicity threshold for humans is also not sufficiently low and should take the entire spectral distribution (SPD) into account, because both studies confirmed that red light can modulate the negative effects of short-wavelength light. Therefore, for prevention, it is crucial to expose ourselves to daylight and use light sources with a balanced spectral distribution and sufficient red light emission during the day, even at low intensities.
Author’s Note
This article is not intended to scare readers. Its purpose is to inform and emphasize how important it is to be exposed to natural sunlight, which has a balanced spectrum. However, since we spend a tremendous amount of time indoors, it is worth considering which light sources we choose to use during the day. To support and synchronize circadian rhythms, we need to use full-spectrum sources with sufficient emission in the melanopic range (455-490 nm) during the day, and for modulating the potential harmful effects of short wavelengths with prolonged and regular exposure to this light, we need sufficient red light emission. Incandescent and halogen bulbs and LEDs with reduced blue content are suitable, especially in the evening, because they do not contain enough energy to stimulate activity and cognitive performance.
Mgr. Tereza Ulrichová, Spectrasol
References:
1) A. Françon, F. Behar-Cohen, a A. Torriglia, „The blue light hazard and its use on the evaluation of photochemical risk for domestic lighting. An in vivo study“, Environment International, roč. 184, s. 108471, february 2024, doi: 10.1016/j.envint.2024.108471.
2) A. Françon et al., „Phototoxicity of low doses of light and influence of the spectral composition on human RPE cells“, Sci Rep, roč. 14, č. 1, s. 6839, march 2024, doi: 10.1038/s41598-024-56980-9.
Images:
Introductory image: F. Behar-Cohen et al., „Light-emitting diodes (LED) for domestic lighting: any risks for the eye?”, Prog Retin Eye Res, roč. 30, č. 4, s. 239–257, july 2011, doi: 10.1016/j.preteyeres.2011.04.002.
Obr. 2: S. Yang, J. Zhou, a D. Li, „Functions and Diseases of the Retinal Pigment Epithelium“, Frontiers in Pharmacology, roč. 12, july 2021, doi: 10.3389/fphar.2021.727870.
Translated using AI